When it comes to foot care, not all pedicures are created equal. While some just want a bit of colour on their toes, for those looking for more than just aesthetic improvement, medical pedicures performed by a podiatrist (who specialises in them) is an experience that leaves you feeling safe and secure about your foot health. Yes, this type of pedicure is well known not only for its ability to improve the appearance of the nails (even without using polish), but also to address a range of other foot-related health issues (pertaining to the nails and skin on the feet). Where others just put a cosmetic bandaid over the problem, we go a lot further to see what we can do to help prevent your concerns from returning, as well as addressing them on the day. Whether you are managing diabetes, suffering from nail disorders, or simply looking to maintain optimal foot health, understanding the importance and benefits of a professional medical pedicure is essential.
What is a Medical Pedicure?
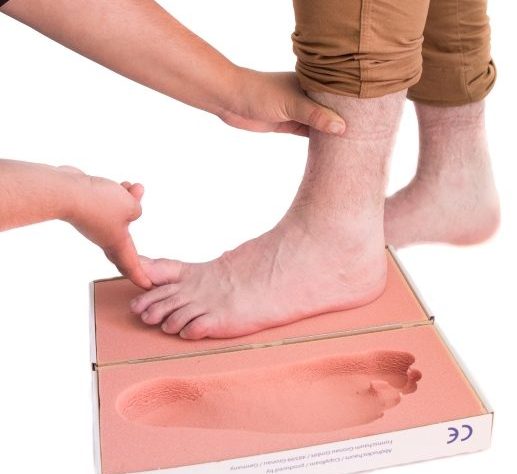
A medical pedicure is a specialised foot care service performed by qualified podiatrists. Unlike a regular pedicure that focuses solely on cosmetic improvements, a medical pedicure targets the long-term health of your feet. During your service, your feet are first thoroughly examined to detect any underlying issues such as fungal infections, ingrown toenails, or excessively dry and cracked skin.
Your podiatrist will then get started using tools that are not only effective and of very high medical quality, but are sterilised and used in an environment that prioritises safety and hygiene. This aspect is particularly important for those with health conditions like diabetes, where maintaining impeccable foot hygiene is a key part of preventing serious complications.
One of the most important parts of medical pedicures is also the education component, in that our team provides comprehensive advice about how you can best support your foot health going forwards. We have just one pair of feet to last us a lifetime, so it’s always important to take the very best care of them.
Nail Restoration Addition To Medical Pedicures
As of 2024, we’re also proud to offer an ‘add on’ option to our medical pedicures with Keryflex nail restoration. Keryflex transforms toenails in one appointment from looking discoloured and damaged (or however your nails are looking now in their current state) to being clear and healthy-looking. It does this by creating an artificial nail over the existing nail that looks, feels and acts like a real nail. What we love is that it doesn’t cause any damage to the nail beneath, and it lets the original nail grow out while looking great.
Keryflex nails are light, flexible and natural – so they move naturally with the toes instead of rigid, damaging alternatives that you may find at a salon. The nail is non-porous and doesn’t allow moisture to penetrate between the natural nail and the Keryflex nail. This means it won’t irritate or cause further damage, and it won’t exacerbate any existing fungal nail infections or other conditions that you may have. In fact, Keryflex contains an antifungal (Piroctone Olamine) to help interfere with the growth of existing fungal infections. Read more about Keryflex here.
Best Medical Pedicure Clinic In Auckland
Here at Perform Podiatry, we take great care in offering high-quality medical pedicures that consider your range of foot health needs and priorities. With us:
- Your medical pedicure is always completed by only qualified, registered and experienced podiatrists
- You can feel safe knowing we uphold the highest standards of hygiene.
- You know we go above and beyond from our 250+ reviews on Google that give us a 5-star average
- If during your appointment we uncover other foot ailments or problems (like plantar warts), you know you’re in the best hands and place to have this treated too
- We’re conveniently located inside the One Health building on Remuera Road
What to Expect During Your Visit
When you first enter the clinic, we’ll start with a consultation so your podiatrist is fully informed as to why you’ve come to see us, your medical history, all about any foot concerns you have or any changes you’ve noticed, and the like. This assessment helps identify any specific issues that need special attention – including any ones that you may not have picked up on.
We’ll then start by trimming your toenails using our German-made and individually steam-sterilised nail clippers, reducing any hard areas of dry, dead callused skin, removing any corns from the feet and toes, treating and reducing any cracks in the heels, and managing similar problems using a surgical-grade scalpel.
We make sure to remove any skin, dirt and anything else trapped beneath or down the sides of the nail with a sterilised file. When this build-up is allowed to remain, you can experience discomfort, pressure, and you may be more vulnerable to infection. Part of your treatment uses a precision burr to reduce the thickness of the nails where needed, while smoothing the ridges of the nails and removing overgrown cuticles and jagged nail ends. All our burrs are steam-sterilised and we have a large variety of different sizes, shapes and materials for each purpose – whether it be reducing a very thick, crumbly nail or polishing a delicate, thin nail.
Your dry, flaky and uneven skin will be smoothed and reduced and a disposable nail file is used to smooth out any final edges that may catch on your socks or stockings. The nails are then cleaned with a clear antiseptic spray, followed by tea tree oil – a natural antifungal and anti-bacterial. Finally, we apply the appropriate moisturiser to your feet to make you feel great on your feet.
Aftercare and Maintenance
Giving you the right information to support your foot health for the long-term is a key part of what we do here at Perform Podiatry. We’ll advise you on the best things you can be doing for your specific circumstances, which may include:
- Regularly applying a foot-specific moisturiser to help keep your skin soft and prevent cracks or dryness.
- Keeping your toenails trimmed straight across to avoid issues like ingrown toenails. Also, avoiding cutting too close to the skin.
- Choosing shoes that fit well and provide adequate support. Avoiding tight shoes that could cause pressure points or contribute to foot deformities.
- Regularly inspecting your feet for any changes or signs of problems, especially if you have diabetes or other conditions that affect foot health.
- Scheduling follow-up visits as recommended by your podiatrist to keep your feet in optimal condition and prevent future issues.
FAQs
Is a medical pedicure covered by health insurance?
Your coverage will vary depending on your health insurance policy and the nature of the treatment. We highly recommend checking in with your insurance provider for specific details regarding your coverage prior to booking your appointment as we don’t have access to any information about your specific policy.
How often should I get a medical pedicure?
The frequency depends on your specific foot health needs. Generally, a medical pedicure every 6 to 8 weeks is sufficient for maintaining healthy feet, but your podiatrist may recommend a different schedule based on your conditions. Some people stretch their appointments out to 16 weeks, and others come in every 4 weeks if their toenails or corns grow quickly and they have a difficult time managing them otherwise.
Can anyone have a medical pedicure?
Yes, medical pedicures are suitable for most people, especially those with specific foot health concerns or conditions like diabetes. They are also greatly beneficial for elderly individuals who might struggle with foot care at home.
What should I bring to my medical pedicure appointment?
You don’t need to bring anything specific to your appointment, though we do ask that you remove your nail polish before coming in.





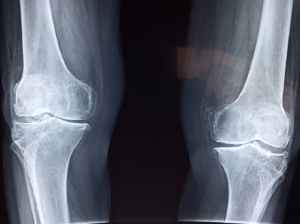 Learning that you have fragile bones can be concerning, and for many, leave them with a lot of questions:
Learning that you have fragile bones can be concerning, and for many, leave them with a lot of questions:
 While medical pedicures are a favourite with our patients, there are more ways that we work with our patients to help them on the slopes, including:
While medical pedicures are a favourite with our patients, there are more ways that we work with our patients to help them on the slopes, including: 
 Yes, you should. Every toe bone break is different – some are more severe than others, and there are special considerations based on which toe you’ve broken and what kind of a break it is, as well as your physical health and medical conditions.
Yes, you should. Every toe bone break is different – some are more severe than others, and there are special considerations based on which toe you’ve broken and what kind of a break it is, as well as your physical health and medical conditions.