
You’ve had heel pain before and were ecstatic when it
finally went away. Weeks, or even months, of taking it easy, wearing the right shoes and orthotics, doing the right stretches and following the sound advice of your Podiatrist had paid off. You were able to hit the ground running, literally, without that gnawing pain, dull aches or any discomfort. Life was back to its happy, healthy self.
So what changed and why is the pain back?
Let us first assure you that pain doesn’t come back for no reason or without a cause. It’s also not a case of that it never healed in the first place. Your injury was indeed completely healed if you were able to resume life and daily activities without pain or symptoms. And it can be completely healed again.
However.
Just like how we can throw a ball through a window, repair the window, and throw a ball through it again, we can re-injure the same muscle, tendon, or ligament twice. But this time, there’s usually more to it.
When you sustain an injury for the first time, there’s a good chance it could be an unfortunate wrong-time, wrong-place injury. You ran too fast for the ball, tripped over, and
snap. Or you went for a 12-hour hike for the first time, something you’re likely never to do again, and your feet flared up from injury. In cases like these, and most accidents, as Podiatrists we look at managing your symptoms, relieving your pain, and helping you get better and heal as fast as possible.
But when an injury re-occurs, that’s a red flag for us to further investigate whether there is something else, either intrinsic (to do with your bones, joints, muscles, tissues) or extrinsic (to do with your footwear, with a sport you play and factors outside of your body) that is causing or contributing to your injury.
Usually, there is a cause we can control
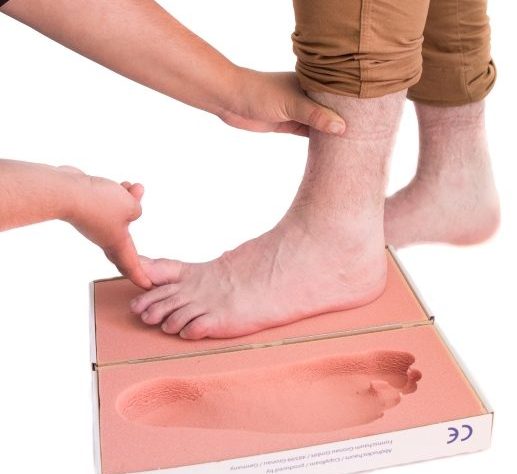
This is why it’s important for us to conduct a comprehensive biomechanical assessment. A biomechanical assessment looks at:
- Your foot posture
- Muscle strength
- The range of motion through the joints of your feet
- The way you walk (gait analysis)
- Structural abnormalities
- Footwear assessment
- Various other tests depending on the findings
From this, we can deduce likely causes for your heel pain and tissue damage. If you have flat feet, wear footwear with relatively low support, occasionally run and get plantar fascial heel pain, it is likely that the repetitive strain on your fascia from running without support is causing damage and leading to pain. Or it could be that you’re getting the same pain at the back of your heel during soccer season again, when you’re training lots and wearing the same soccer boots that have a low-set heel. These boots will put greater strain on the insertion of your achilles tendon and paired with strenuous activity, can definitely overuse and damage your achilles tendon leading to heel pain.
Treating the cause, not just the symptoms
In these cases and so many more, it’s not just about treating your existing symptoms, but putting appropriate measures into place to stop the pain from coming back.
This is one of our key focuses here at
Perform Podiatry – preventing re-injury so it won’t keep bothering you in the future. We offer comprehensive biomechanical assessments from expert Podiatrists that specialise in Sports Medicine and Clinical Biomechanics. We’re proud to be trusted by hundreds of patients each month to help them feel great and perform at their best.
We often use
orthotics to control the movement of the feet and reduce the strain on otherwise overused and tired muscles. We also use strengthening techniques to get you back to your best.
If your injuries keep coming back or you’re experiencing any issues with your feet or legs, give us a call on
09 523 2333 and one of our friendly team will be happy to answer any questions you may have!

 A lot of us have heard that it’s not uncommon to have a slight difference in the size of our feet or even legs. We often advise patients to buy shoes to the size of the larger foot so that toes don’t get cramped and cause pain. But when it comes to having a slight difference in the length of the legs, does it make any difference or have any effect on the body? Let’s start with the basics about limb length discrepancies.
A lot of us have heard that it’s not uncommon to have a slight difference in the size of our feet or even legs. We often advise patients to buy shoes to the size of the larger foot so that toes don’t get cramped and cause pain. But when it comes to having a slight difference in the length of the legs, does it make any difference or have any effect on the body? Let’s start with the basics about limb length discrepancies.
