Corns and callus are a big problem for many of our patients here at Perform Podiatry. Unfortunately, they’re often a problem that goes untreated for far too long and causes much unnecessary pain, that can otherwise be relieved instantly – in just a single appointment!
We were inspired to write this by two patients that came in first thing today, one after the other. The first has corns that she gets taken care of regularly, so they never build up enough to cause her pain. The second patient hadn’t seen us in over a year as life had become busy and she just put off making those little maintenance appointments – which is totally understandable – until she realised that her corn had started causing her quite a fair bit of pain!
So, what causes corns and callus and why do they develop?
The answer to the cause is
friction and
pressure. It’s the rubbing or excess pressure (usually from walking) on an area of the foot that’ll lead to the development and longevity of the corn. We joked with a patient this morning that if you were to stop walking, then your corns wouldn’t come back, because of their direct result from excess pressure. However, we’re also all busy people that rely on our feet to get us
everywhere so that’s not an option just yet.
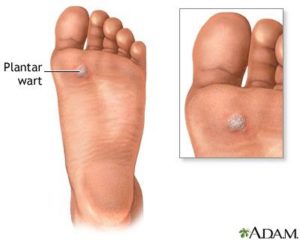
The reason you’ll develop a corn on the bottom of your foot but your walking buddy won’t, however, is also largely related to your foot biomechanics. Of course, there are other factors at play like your footwear, the type of ground you walk or run on, and many more. But most likely, it’ll be that a bone in your foot is sitting that little bit lower than the others – and not because of anything you’ve done – and there’ll be a lot more pressure on that bone with every step you take. Next minute, you’ve got a corn.
And why are some corns painful and not others?

Corns (and callus) is really just a build-up of hard, dead skin. It’s actually a protective mechanism from your body – think about it like this: There’s an area of your foot that is constantly undergoing a
lot of pressure. Your body thinks ‘
If I don’t do anything to protect this normal skin, it might tear/break/wear down and I’ll be susceptible to infection’. So the skin hardens. You develop protection from the regular pressure.
But then…
It keeps building to the point that it feels like you’re walking on a pebble with every step. The thick mass irritates the regular skin around it. It becomes tender and may redden. It becomes too big, and now uncomfortable and painful.
Here we have identified the sweet spot… You’ve got to manage your corns and callus before they get to that painful point. And as podiatrists, that’s something we can do very easily for you. Just like this corn below – just one appointment and boom, the pain is gone. It really is that simple!
To get rid of the corns, we use a scalpel very skillfully to debride the thickened skin. Because it’s just hard, dead skin, you don’t feel a thing. What you do feel is a feeling of relief as you place your feet back on the ground and no longer feel that painful lump. Success!
If you or any of your family is suffering from painful or uncomfortable corns and callus, don’t hesitate to get in touch with us here at Perform Podiatry. There’s nothing better for us as practitioners than to see patients who initially came in with painful feet walk out feeling great and pain-free. It’s why we love what we do!
To book in with our fantastic practitioners, you can give us a call on
09 523 2333 or
book online here.


 Splinters can be caused by a range of things – a prickle from a plant, a shard of glass, a wood splinter and more. As they are a ‘foreign’ object that pierces and enters the skin, aside from being very painful, they can also contain bacteria that can cause an infection if the splinter isn’t removed. This is why splinters
Splinters can be caused by a range of things – a prickle from a plant, a shard of glass, a wood splinter and more. As they are a ‘foreign’ object that pierces and enters the skin, aside from being very painful, they can also contain bacteria that can cause an infection if the splinter isn’t removed. This is why splinters 

 Corns (and callus) is really just a build-up of hard, dead skin. It’s actually a protective mechanism from your body – think about it like this: There’s an area of your foot that is constantly undergoing a lot of pressure. Your body thinks ‘If I don’t do anything to protect this normal skin, it might tear/break/wear down and I’ll be susceptible to infection’. So the skin hardens. You develop protection from the regular pressure.
But then…
It keeps building to the point that it feels like you’re walking on a pebble with every step. The thick mass irritates the regular skin around it. It becomes tender and may redden. It becomes too big, and now uncomfortable and painful.
Here we have identified the sweet spot… You’ve got to manage your corns and callus before they get to that painful point. And as podiatrists, that’s something we can do very easily for you. Just like this corn below – just one appointment and boom, the pain is gone. It really is that simple!
To get rid of the corns, we use a scalpel very skillfully to debride the thickened skin. Because it’s just hard, dead skin, you don’t feel a thing. What you do feel is a feeling of relief as you place your feet back on the ground and no longer feel that painful lump. Success!
If you or any of your family is suffering from painful or uncomfortable corns and callus, don’t hesitate to get in touch with us here at Perform Podiatry. There’s nothing better for us as practitioners than to see patients who initially came in with painful feet walk out feeling great and pain-free. It’s why we love what we do!
To book in with our fantastic practitioners, you can give us a call on
Corns (and callus) is really just a build-up of hard, dead skin. It’s actually a protective mechanism from your body – think about it like this: There’s an area of your foot that is constantly undergoing a lot of pressure. Your body thinks ‘If I don’t do anything to protect this normal skin, it might tear/break/wear down and I’ll be susceptible to infection’. So the skin hardens. You develop protection from the regular pressure.
But then…
It keeps building to the point that it feels like you’re walking on a pebble with every step. The thick mass irritates the regular skin around it. It becomes tender and may redden. It becomes too big, and now uncomfortable and painful.
Here we have identified the sweet spot… You’ve got to manage your corns and callus before they get to that painful point. And as podiatrists, that’s something we can do very easily for you. Just like this corn below – just one appointment and boom, the pain is gone. It really is that simple!
To get rid of the corns, we use a scalpel very skillfully to debride the thickened skin. Because it’s just hard, dead skin, you don’t feel a thing. What you do feel is a feeling of relief as you place your feet back on the ground and no longer feel that painful lump. Success!
If you or any of your family is suffering from painful or uncomfortable corns and callus, don’t hesitate to get in touch with us here at Perform Podiatry. There’s nothing better for us as practitioners than to see patients who initially came in with painful feet walk out feeling great and pain-free. It’s why we love what we do!
To book in with our fantastic practitioners, you can give us a call on