We love seeing kids here at Perform Podiatry. Partly because it’s hard to be away from our own and they brighten up our day, but largely because of the massive difference that we know we can make to their lives and development.
Kids should be able to run, play, explore, learn and have fun without being limited by pain or held back by foot or leg dysfunction. Thankfully, issues that arise in kids are usually much easier to manage than in adults. Today we thought we’d share on a condition that we’ve had a few questions about lately from concerned parents – knock knees!
What are knock knees?
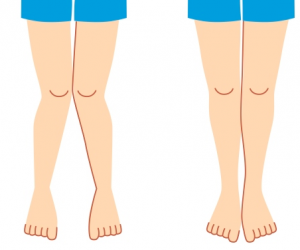
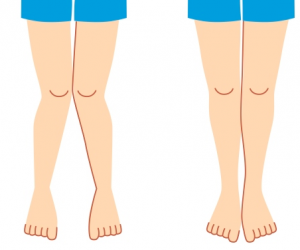
Knock knees, medically referred to as genu valgum, is the position of the knees where they are turned inwards toward one another, meaning they ‘knock’ or brush against one another as you walk. It’s often seen in children between the ages of 3 and 5, and helps them maintain balance as they develop their walking.
What causes knock knees?
Before you panic – don’t worry. Knock knees are usually a normal variation of growth and development, and this position is just how some children find their footing. However. They also may be an indicator of an underlying condition such as rickets or osteomalacia. In these cases, knock knees may not develop until the child is six years old, or persist after the age of 8.
Generally speaking, contributing factors to the development of knock knees can include:
- Obesity
- Loose ligaments at the knees that place excess pressure on the knee joints
- Infection or injury to the knee or shin bone (tibia)
- Conditions that affect bone development
- Calcium or Vitamin D deficiency
If you’re worried, it’s always a good idea to get your child checked. This way we can inform you if your child has a normal or abnormal variation of knock knees, as well as track their progress over time to ensure that the lower limbs are developing appropriately.
What are the symptoms?
The inward bending of the knees is the biggest symptom. You’ll also notice a gap between the ankles when the knees are together. One knee may turn inwards more than the other and pain isn’t typically experience during young childhood years. Where knock knees continue beyond the childhood years, symptoms may include:
- Knee pain
- Limping or altered walking patterns
- Stiffness in the knee joints
- Increased risk of developing knee arthritis
What should you do?
Because knock knees can resolve by the age of 7, you may wish to wait and see, or you may wish to get your child checked by your podiatrist. Your podiatrist will be able to assess exactly what is happening with the knee position, as well as the hip and foot position as these will be affected to some extent as a result.
If your child is experiencing any painful symptoms, interventions such as orthotics, bracing, stretching and strengthening may be used to relieve the symptoms – as kids shouldn’t be in pain from their knee position, and if this is the case, it’s likely causing other problems too.
Where knock knees persist into adulthood, management needs to be aimed at the issues that this misalignment is creating as opposed to the knee position itself. In later years, it is also important to rule out the possibility of any underlying bone conditions. Your podiatrist will be able to create a tailored management plan based on the symptoms you’re experiencing and your history.
If you’re concerned about your kid’s feet or legs, or just want that peace of mind that everything is developing normally, give our expert team a call on
09 523 2333 or book online!

 We love seeing kids here at Perform Podiatry. Partly because it’s hard to be away from our own and they brighten up our day, but largely because of the massive difference that we know we can make to their lives and development.
Kids should be able to run, play, explore, learn and have fun without being limited by pain or held back by foot or leg dysfunction. Thankfully, issues that arise in kids are usually much easier to manage than in adults. Today we thought we’d share on a condition that we’ve had a few questions about lately from concerned parents – knock knees!
We love seeing kids here at Perform Podiatry. Partly because it’s hard to be away from our own and they brighten up our day, but largely because of the massive difference that we know we can make to their lives and development.
Kids should be able to run, play, explore, learn and have fun without being limited by pain or held back by foot or leg dysfunction. Thankfully, issues that arise in kids are usually much easier to manage than in adults. Today we thought we’d share on a condition that we’ve had a few questions about lately from concerned parents – knock knees!