
Excruciating pain in one of your toes? Wondering whether you’ve broken it – and if you have – whether you should go to the hospital or a doctor or a podiatrist and what they’ll do?
Broken toes are more common than many people realise – and unfortunately, so is suspecting a broken toe, not doing anything about it, and then putting up with the consequences afterwards. While New Zealand tends to have a strong she’ll be right mentality, broken toes are not something that should be shrugged off in the hopes that the problem will just go away and be good as new.
Here’s the inside scoop about broken toes and what they really mean for you.
What does a broken toe feel like?
Broken toes feel painful, swollen and may have some purple bruising from the bleeding beneath the skin. You may get some numbness or tingling, have marked redness or streaking around the toe, and your toe may look crooked or out of place. Try standing with weight and pressure on your forefoot and toes at least a few hours after the pain begins. Can you do so comfortably or are you unable to bear weight without significant pain on the toe? If it’s the latter, it very well could be broken. If it’s the former, don’t rule out the break just yet – some are more subtle than others!
How can toes become broken?
The most common ways people tend to break their toes are from stubbing it, dropping something on it, and during contact sports – particularly falls and tackles.
Should I see someone for my broken toe? Who?
 Yes, you should. Every toe bone break is different – some are more severe than others, and there are special considerations based on which toe you’ve broken and what kind of a break it is, as well as your physical health and medical conditions.
It’s important that your feet are also checked for circulation and nerve damage, skin injuries and any resultant wounds, as well as any injuries to any bones, joints, ligaments and tendons around the area. Often, breaks don’t happen on their own, and you’ll need to address any related problems too if you’re going to recover effectively.
Your podiatrist should be the first port of call due to their comprehensive knowledge of the feet. They’ll be able to assess your toe against other causes of toe pain to get a clearer diagnosis. They can also refer you for an x-ray to confirm the break.
Yes, you should. Every toe bone break is different – some are more severe than others, and there are special considerations based on which toe you’ve broken and what kind of a break it is, as well as your physical health and medical conditions.
It’s important that your feet are also checked for circulation and nerve damage, skin injuries and any resultant wounds, as well as any injuries to any bones, joints, ligaments and tendons around the area. Often, breaks don’t happen on their own, and you’ll need to address any related problems too if you’re going to recover effectively.
Your podiatrist should be the first port of call due to their comprehensive knowledge of the feet. They’ll be able to assess your toe against other causes of toe pain to get a clearer diagnosis. They can also refer you for an x-ray to confirm the break.
Can I treat my broken toe at home myself?
You can get some temporary pain relief at home by using ice to help reduce the swelling, keeping your foot elevated, removing any weight and pressure from the foot, changing to open-toed footwear, and using non-steroidal anti-inflammatories like nurofen. But you still need to see your podiatrist as quickly as possible. When broken toes aren’t allowed to heal properly or in the right position, this can have damaging consequences for you further down the line, from a prematurely arthritic joint to crooked toes, painful high-pressure areas or altered gait. At its worst, you may end up needing surgery – which may have been preventable. This is why it’s always best to get help early.
How are broken toes treated?
If you have a straightforward break where the bone is still well aligned, then your treatment may involve anything from ‘buddy taping’ the toe to act as a splint and then offloading the area, to using a moon boot for full immobilisation. You may need to change your footwear while your toe heals to give it adequate space and avoid harmful pressure.
Here at Perform Podiatry, we understand that an effective treatment plan is far more complex than saying don’t walk on this foot for the next four to six weeks. Every treatment plan is made following a comprehensive assessment, and importantly, getting to know you, your work and life situation, and discussing which treatment options will be best for you under your circumstances.
Experienced podiatrists in Remuera, Auckland
If you have pain in your forefoot and you’re worried that you’ve broken a toe or sustained another injury, our experienced podiatry team is here to help. We’re located in the One Health building on Remuera Road, with x-ray services available within our building if needed.
Book your appointment online here or call us on (09) 523 2333

Do we trim toenails? Do we correct your foot posture using orthotics? Do we remove your corns? Do we help correct bunions? The answer is a big yes to all of the above – and a whole world more.
Every once in a while, we’re reminded that for those that have never been to a podiatrist, or only had one specific problem treated, they have no idea about the number of people with a variety of conditions that we help every year. So today, we’re sharing ten of the many problems that you may not have known that we can help you with.
In-toeing in kids
While in-toeing, as well as out-toeing, can be a normal variation when kids are first learning to walk, if in-toeing persists into the primary school years, or if it’s causing kids to trip, fall, be unable to keep up with their friends or causing them pain, they may need a little help with straightening their feet. This is something we absolutely offer, using an in-shoe device called a gait plate that your child won’t even notice! This is combined with some easy and child-friendly exercises to help kids walk straight and feel great on their feet.
Foot drop
Foot drop describes a situation where the forefoot drops down instead of being able to be lifted up to clear the ground. This can be incredibly frustrating for those affected, causing regular tripping with normal gait, or having to lift the knee at the hip to try to compensate, which may lead to pain at the hip, knee or glutes. We use specialised braces that are lightweight, modern and can often fit conveniently inside footwear, these prevent the foot from dropping down and help you clear the ground.
Bunions
Bunions describe the bony bumps that develop on the side of your big toe (or little toe!) that make it difficult – and possibly painful – for you to fit shoes properly. We can help with both encouraging the toes to straighten, as well as preventing or at least slowing the bunions from worsening. We have a number of treatments to try for this – and none of them involves surgery.
Falls & instability
Feeling unstable and unconfident on your feet is scary – both inside and outside of the house. We get to the cause of your instability, selecting the best strategies and treatments to help promote stable and confident gait. Whether it’s from years of repeated ankle sprains that have left you with chronic ankle instability, an accident and subsequent surgery that has restricted the movement on your feet, or it’s a condition or disease that has left you feeling less stable, we will work with both your lower limbs and your footwear to help you walk and feel your best.
Poorly fitting footwear
Have good shoes you love but that don’t quite fit properly anymore? Whether it’s a bunion, an altered foot shape following an accident or something else, we’re one of the only clinics in Auckland that offer shoe stretching where appropriate.
Curly and overriding toes
Toes that are clawed or positioned over one another aren’t just an aesthetic problem – their position makes it difficult to fit comfortably into shoes, and puts you at risks of corns, callus, trapping moisture between the toes that may break down the skin, and much more. We can help by creating custom devices for the toes that will keep them separated and in a better position for regular foot function – and your comfort. We’ll also manage any corns, callus or wounds that have developed as a result of the position.
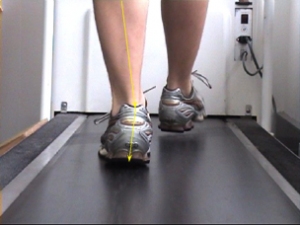
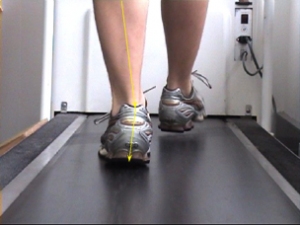
Retraining your gait (the way you walk and run)
The way you’ve learnt to walk and run can impact your energy output, performance, injury risk and more. We can help you retrain your gait by identifying your current patterns on the treadmill, prescribing stretching and strengthening exercises to help with any insufficiencies, and teaching you different techniques to promote healthy gait patterns.
Managing ulcer risk
Ulcers are one of the leading causes of lower limb amputations aside from Trauma. Whether you’ve recently discovered an ulcer or you’ve had one that hasn’t healed on its own for months, we offer wound care services to manage and monitor your ulcer, and help prevent it from causing you serious complications and side effects. We debride any build-up around the wound where safe and clinically appropriate, have a range of specialised dressings to offer the right level of moisture support and will help you offload the ulcer in a variety of ways. This might be using pads with your dressings or creating specialised orthotics (foot inserts) that have a cut-out or drop-down in the precise location of your ulcer, so that you stop applying pressure to it with every step you take in your shoes. We relay our findings and management plan to your GP and any other health professionals that you request, so we all work as a unified team to help get the best outcomes for your health.
Fungal nail infections
Fungal nail infections can be difficult to treat for so many reasons. Some studies have shown that up to 50% of people who thought that they had a fungal nail infection actually didn’t – their nails were being affected by something else instead! This is why we offer in-clinic testing to confirm that the discolouration and other symptoms in your nails are being caused by a fungus. This simple test takes about 5-10 minutes and is performed by our podiatry team. From there, we can recommend the best anti-fungal treatment and teach you our tips for not just getting rid of the fungal nail infection – but keeping it gone in the future.
Foot & leg pain
Okay, so this one we know the majority of you probably already know that we treat – but given that foot and leg pain is one of the most common things we manage on a daily basis, it’s definitely worth a mention! From heel pain like plantar fasciitis, to Achilles pain, shin splints, knee pain, toe pain and so much more, this is one of our areas of special interest that we know inside out and love helping you with!
Can’t see your problem on the list?
Don’t worry! We offer many more services, including medical pedicures, ingrown toenail surgery, sports medicine and much more. Check out our range of services on our website – or just give us a call and let us know your problem – we’ll be happy to either book you in or point you in the right direction if we’re unable to help with your specific problem.
Book your appointment online here or call us on 09 523 2333

Orthotics can be fantastic devices. Like glasses that help us see and perform our best each day, orthotics work to alter the way our feet, muscles and bones move with the goal of optimising our overall function and reducing pain, excess pressure and unnecessary fatigue.
Unlike glasses, however, that do not come into direct contact with our eyes, the daily force placed on the orthotic can cause them to wear out over time. While this is not new information and is (or at least should be) detailed by your Podiatrist when discussing orthotics, it is something that can be easily forgotten or taken for granted when your foot pain is gone and you’re performing well – until your pain quickly returns and you’re not sure why.
To put things in perspective, here are 3 quick reasons why you should be seeing your Podiatrist for an orthotic check every year – or two at most.
1. Regardless of how long you’ve had them, your orthotics are working every day.
 Whether you realise it or not – your orthotics are constantly under a lot of pressure. To be precise, you’ll be exerting at least all your body weight over both orthotics – and when you’re running, this can increase to 3 – 4 times your body weight.
Gradually, this can lead to the wear down and compression of your orthotic materials, which affects their ability to provide the support, control and function that they were designed to – and initially would have.
Just like how you’d sharpen a blunt knife so it could keep working effectively, it’s important to check that your orthotics are still doing their job. If they’re not, it doesn’t mean that you’ll always need a completely new set of orthotics. Sometimes, it’s simply a matter of replacing the top cover, reinforcing the control of your orthotics or replacing your pad or addition. You won’t know until you have them checked – and it can be as quick and easy as a 15min check appointment!
Whether you realise it or not – your orthotics are constantly under a lot of pressure. To be precise, you’ll be exerting at least all your body weight over both orthotics – and when you’re running, this can increase to 3 – 4 times your body weight.
Gradually, this can lead to the wear down and compression of your orthotic materials, which affects their ability to provide the support, control and function that they were designed to – and initially would have.
Just like how you’d sharpen a blunt knife so it could keep working effectively, it’s important to check that your orthotics are still doing their job. If they’re not, it doesn’t mean that you’ll always need a completely new set of orthotics. Sometimes, it’s simply a matter of replacing the top cover, reinforcing the control of your orthotics or replacing your pad or addition. You won’t know until you have them checked – and it can be as quick and easy as a 15min check appointment!
2. If your orthotics helped alleviate your original symptoms – how would it affect your life if they came back?
Orthotics are not an ‘on-the-whim’ purchase. They’re a medical device and an investment into your health and mobility for the years to come. They have a very specific function that was prescribed and created by a foot health professional with years of experience in relieving symptoms and improving quality of life. This function may be to stop your foot rolling in and flattening so much, as it was irritating your posterior tibial tendon or plantar fascia and causing pain down the inside of your foot and ankle or the heel. It may be to provide additional stability to your foot and ankle as you’d suffered repeated ankle sprains and had developed some chronic ankle instability along the way. It may have been because your high-arched foot was lacking the shock absorbing function it needed to keep your feet from feeling sore and tired after a long shift on your feet.
Whatever the function – if your pain was alleviated (or at least significantly reduced in the case of arthritic pain) by your orthotics, then there’s a good chance that without the adequate support and control from your orthotics, that this pain can come back. And it’s not only the pain that comes back.
Pain happens for a reason. It’s a sign that something is wrong – that an injury has occurred – and the pain is a by-product of the damage. When your pain comes back, it means an injury has again occurred and that’ll take time to heal and for the pain to go, even after you repair or replace your orthotics. And that can take a significant toll on your quality of life!
3. Your foot structure and position, along with your bone and muscle strength and function, change over time. Your orthotics may need to too.
 As with everything in our lives, we are always changing – and so are our bodies. Our muscles may grow stronger or weaker. Certain medications or events may affect our tissues and the way they function. Our feet change, but they do so very gradually, at a rate that we may not be able to notice. So while we may presume that our feet are the same today as they were 3 years ago, there’s only one way to find out – and that’s to have them checked!
When you come in for an orthotic check, we assess the function of your orthotics against both the reason you needed your orthotics in the first place, and against your feet in their current state. The ultimate question that we look to answer is:
As with everything in our lives, we are always changing – and so are our bodies. Our muscles may grow stronger or weaker. Certain medications or events may affect our tissues and the way they function. Our feet change, but they do so very gradually, at a rate that we may not be able to notice. So while we may presume that our feet are the same today as they were 3 years ago, there’s only one way to find out – and that’s to have them checked!
When you come in for an orthotic check, we assess the function of your orthotics against both the reason you needed your orthotics in the first place, and against your feet in their current state. The ultimate question that we look to answer is:
“are your orthotics in their current state effectively supporting and controlling your feet in their current state?”
If the answer to this question is yes, then that’s fantastic! It’s exactly what we want. If the answer to this question is no, then we’ll figure out why (is it your feet, is it the orthotics, are there other influencing factors like your footwear) and discuss with you the best ways to correct this so you can stay happy, healthy and active for the foreseeable future.
Need that orthotic check after all?
Easy – just book in using our free online booking form here, or give our team a call on 09 523 2333 and book in your appointment. We hope that you’ve been feeling great and performing well – and hope to see you soon!
 Yes, you should. Every toe bone break is different – some are more severe than others, and there are special considerations based on which toe you’ve broken and what kind of a break it is, as well as your physical health and medical conditions.
It’s important that your feet are also checked for circulation and nerve damage, skin injuries and any resultant wounds, as well as any injuries to any bones, joints, ligaments and tendons around the area. Often, breaks don’t happen on their own, and you’ll need to address any related problems too if you’re going to recover effectively.
Your podiatrist should be the first port of call due to their comprehensive knowledge of the feet. They’ll be able to assess your toe against other causes of toe pain to get a clearer diagnosis. They can also refer you for an x-ray to confirm the break.
Yes, you should. Every toe bone break is different – some are more severe than others, and there are special considerations based on which toe you’ve broken and what kind of a break it is, as well as your physical health and medical conditions.
It’s important that your feet are also checked for circulation and nerve damage, skin injuries and any resultant wounds, as well as any injuries to any bones, joints, ligaments and tendons around the area. Often, breaks don’t happen on their own, and you’ll need to address any related problems too if you’re going to recover effectively.
Your podiatrist should be the first port of call due to their comprehensive knowledge of the feet. They’ll be able to assess your toe against other causes of toe pain to get a clearer diagnosis. They can also refer you for an x-ray to confirm the break.



 Whether you realise it or not – your orthotics are constantly under a
Whether you realise it or not – your orthotics are constantly under a  As with everything in our lives, we are always changing – and so are our bodies. Our muscles may grow stronger or weaker. Certain medications or events may affect our tissues and the way they function. Our feet change, but they do so very gradually, at a rate that we may not be able to notice. So while we may presume that our feet are the same today as they were 3 years ago, there’s only one way to find out – and that’s to have them checked!
As with everything in our lives, we are always changing – and so are our bodies. Our muscles may grow stronger or weaker. Certain medications or events may affect our tissues and the way they function. Our feet change, but they do so very gradually, at a rate that we may not be able to notice. So while we may presume that our feet are the same today as they were 3 years ago, there’s only one way to find out – and that’s to have them checked!