Whether you’re in the office or working remotely, a lot of our workforce spends a significant portion of their day sitting at a desk, often in front of a computer. While sitting may seem natural and harmless, poor posture has the potential to lead to various health issues, including discomfort, pain, and musculoskeletal problems that require professional care. Yes, the way you position your hips, legs, and feet when sitting on a chair can significantly impact your overall well-being. Here’s How.
The Consequences of Poor Posture
Your Hips
There are two main elements of poor posture when it comes to the hips. Sitting with a slouched hip posture, where the hips are rolled backwards, can lead to excessive pressure on the lumbar spine. This position places extra strain on the lower back muscles, potentially causing lower back pain and discomfort. Sitting with elevated hips, where your hips are higher than the knees due to an inadequate chair height can result in pressure on your hip flexors. Over time, this can lead to tightness and discomfort in these muscles.
Your Legs
Sitting with your legs crossed can restrict blood flow and lead to numbness and tingling in the legs. It may also place uneven pressure on the knees, potentially contributing to knee pain and long-term joint issues. Similarly, keeping your legs extended straight under the desk can hinder blood circulation, causing discomfort and potentially contributing to varicose veins over time.
Your Feet
Allowing your feet to dangle without proper support can result in lower back pain and poor circulation in the legs. This posture may also lead to the development of varicose veins. Tucking your feet under the chair can also create unnecessary pressure on the knees and lead to discomfort over time.
So How Should You Be Sitting?
Aim to:
- Sit with your hips in a neutral position, where the natural curve of the lower spine is maintained. This minimises the stress on the lower back and helps prevent pain and discomfort.
- Use a chair with lumbar support, as it can help maintain the natural curve of your lower back and provide additional comfort.
- Ideally, keep your hips and knees at a 90-degree angle to one another when sitting. Adjust the chair height so that your feet are flat on the floor, promoting proper circulation and reducing stress on the knees.
- Avoid crossing your legs, instead keep both feet flat on the ground or on a footrest to prevent pressure on the knees and ensure optimal blood flow.
- Use a footrest, as it can help support your feet and maintain proper posture while reducing the risk of lower back pain.
- Ensure that your feet are not tucked under the chair. Instead, keep them flat on the ground or on a footrest.
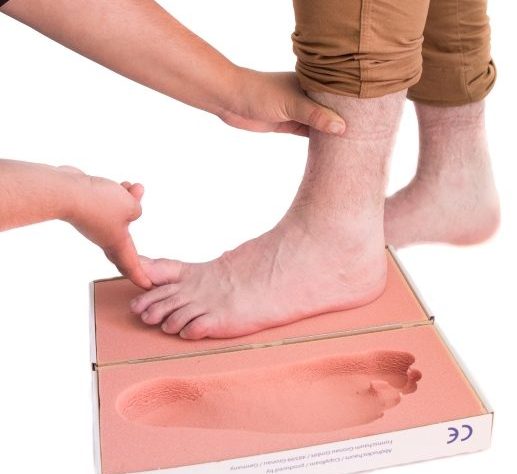
Experiencing Pain In Your Feet Or Legs?
If you’re experiencing pain in your feet or legs, whether that’s related to your lower limb posture or from something else – we’d love to help. Give our podiatry team a call. We’re based in Remuera, in the One Health medical building, close to Newmarket. Call us on 09 523 2333 or book online here.