What causes ulcers?
 Ulcers can occur due to a number of causes, both diabetic and non-diabetic. Often there is an associated medical problem or condition, so it is essential that this is uncovered and treated. Areas of high pressure over bones and joints can contribute to the development of all ulcers. They can be:
Ulcers can occur due to a number of causes, both diabetic and non-diabetic. Often there is an associated medical problem or condition, so it is essential that this is uncovered and treated. Areas of high pressure over bones and joints can contribute to the development of all ulcers. They can be:
- Neuropathic
- Arterial
- Venous
- Pressure-related
What are the symptoms?
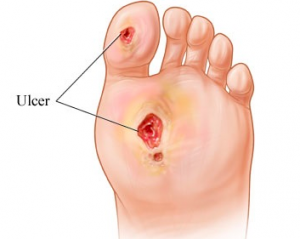
Foot ulcers may be circular in shape or may have distorted edges. They start as a reddened area that blister, peel or crack to create an open wound. They often weep and may have some bloody discharge. The layers of skin become thin and the ulcer may expose bone, muscle or tendon. The edges may become brown/black or stay pink/red. If an infection occurs, the ulcer may have patches of yellow/green and may produce exudate and an unpleasant odour.How are ulcers treated?
Because ulcers put patients at risk of serious complications, it is important that ulcers are treated professionally and effectively. Treatment will depend on the cause of your ulcer and the contributing factors. Because of the often systemic nature of ulcers, treating the cause often involves looking at your overall circulatory issues, venous problems, and the management of diabetes where present. Your podiatrist will be able to:- Debride the ulcer where needed to remove any dead tissue that is impairing the healing and repair process
- Identifying and helping you manage infection where present
- Off-load pressure away from the ulcer through pads, orthotics, footwear or total contact casting
- Liaise with other health professionals in the best management of your ulcers








